Regular screening is important to detect diabetes-related health problems early. It’s also important to keep your waist measurement, blood pressure, blood glucose levels, HbA1c and cholesterol within recommended ranges.
It's very important that you don't smoke if you have diabetes as it increases the likelihood of health problems.
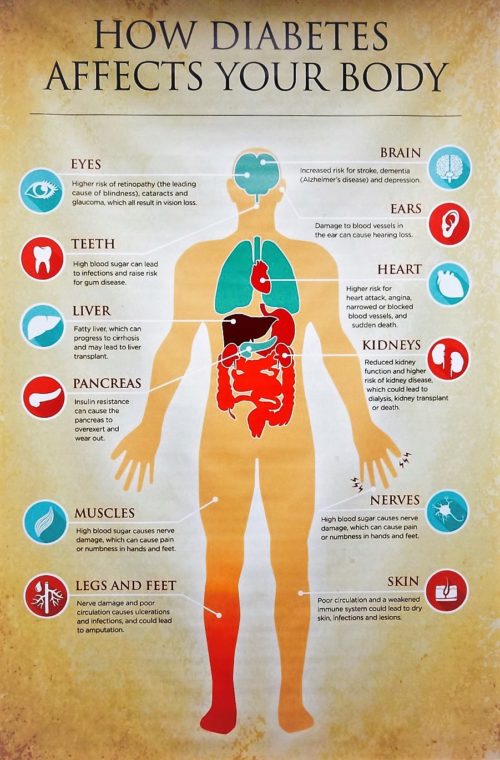
About diabetes – long-term effects
Diabetes is a condition in which there is too much glucose (a type of sugar) in the blood. Over time, high blood glucose levels can damage the body's organs. Possible long-term effects include damage to large (macrovascular) and small (microvascular) blood vessels, which can lead to heart attack, stroke, and problems with the kidneys, eyes, gums, feet and nerves.
Reducing the long-term effects of diabetes
The good news is that you can reduce the risk of the long-term effects of diabetes by keeping blood pressure, blood glucose and cholesterol levels within recommended range. Also, being a healthy weight, eating healthily, reducing alcohol intake, and not smoking will help reduce your risk.
Regular check-ups and screening are important to pick up any problems early.
Diabetes and healthy eating
If you have diabetes it’s important to include a wide variety of nutritious and healthy foods in your diet, and to avoid snacking on sugary foods.
Enjoy a variety of foods from each food group – be sure to include foods high in fibre and low in fat and reduce your salt intake. It’s helpful to consult with a dietitian to review your current eating plan and provide a guide about food choices and food quantities.
Alcohol intake and diabetes
Limit alcohol intake. If you drink alcohol, have no more than two standard drinks per day. If you are pregnant or considering pregnancy or are breastfeeding, then zero alcohol intake is recommended.
Diabetes and healthy weight
If you are overweight, even losing a small amount of weight, especially around the abdomen, helps to lower your blood pressure, blood glucose and cholesterol levels.
It can be difficult trying to lose weight, so to get started set yourself a short-term, achievable goal. Try thinking about the food you are eating, whether you really need it, if it's a healthy choice, and consider the portion size. An accredited practicing dietitian can help you set a realistic meal plan and answer any food related questions you may have.
Diabetes and exercise
Be as active as possible. The Australian physical activity guidelines recommend at least 30 minutes of moderate intensity physical activity a day, and to gradually build up the duration and intensity of exercise. For weight loss, a minimum of 60 minutes a day is recommended.
If you are unable to do physical activity such as walking, swimming or gym work, then consider water aerobics, chair exercises or strength resistance training with light weights.
Check with your doctor if you’re not sure whether the exercise you are planning to do is suitable. If you have a medical condition, it may prevent you from doing certain types of physical activity. An exercise physiologist is a health professional that can help set you up with an exercise plan that will suit your needs and ability.
Smoking and diabetes
Smoking is the greatest single lifestyle risk factor for developing diabetes complications. Smoking can undo all the benefits gained by weight loss, healthy eating, good blood glucose and blood pressure control.
Smoking affects circulation by increasing heart rate and blood pressure, and by making small blood vessels narrower. Smoking also makes blood cells and blood vessel walls sticky and lets dangerous fatty material to build up. This can lead to heart attack, stroke and other blood vessel disease.
People with diabetes who smoke have higher blood glucose levels and less control over their diabetes than non-smokers with diabetes.
Regular diabetes screening checks
You can help pick up problems early by having regular checks of your:
- blood pressure
- blood glucose levels including HbA1c
- cholesterol and triglycerides
- kidney function
- eyes
- feet
- teeth and gums.
Blood pressure checks
Have your blood pressure checked every time you visit your doctor or at least twice a year. It's recommended that your blood pressure is under 130/80. Blood pressure control is just as important as blood glucose control in reducing the risk of diabetes complications.
Blood glucose checks
Keeping your blood glucose levels within the recommended range can help reduce your risk of long-term diabetes-related health problems. Speak to your doctor or diabetes educator if you are unsure what your recommended blood glucose levels are.
Your doctor or diabetes nurse educator may advise you to check your blood glucose levels at home depending on your individual management plan. Regular measuring of your blood glucose levels gives you information about how medicine, food, exercise, illness and stress affect your diabetes.
HbA1c is a measurement of how much glucose has attached to your red blood cells over a three-month period. It is a direct measurement of your risk of long-term diabetes-related health problems.
It’s recommended that you measure your HbA1c levels at least every year, but they may need to be checked every three to six months. Both HbA1c and blood glucose monitoring are important ways to assess your diabetes management.
The goal for HbA1c for most people with diabetes is no more than 53 mmol/mol or 7%. However, recommended ranges can vary depending on the person, for example, with children, frail elderly people, pregnant women, or the type of diabetes and its management.
Cholesterol and triglyceride tests
Have a cholesterol and triglyceride test at least once a year. Aim for total cholesterol less than 4.0 mmol/L and triglycerides less than 2.0 mmol/L.
There are a number of causes of high cholesterol, including your family history and your diet. Too much saturated fat in your diet can increase the LDL (bad) cholesterol in your blood and result in the build-up of plaque in your blood vessels.
Foods high in saturated fats include full-fat dairy products, fatty meats, pastries, biscuits, cakes, coconut cream or coconut milk, palm oil and fatty take-away foods.
Long-term effects of diabetes
The most common long-term diabetes-related health problems are:
- damage to the large blood vessels of the heart, brain and legs (macrovascular complications)
- damage to the small blood vessels, causing problems in the eyes, kidneys, feet and nerves (microvascular complications).
Other parts of the body can also be affected by diabetes, including the digestive system, the skin, sexual organs, teeth and gums, and the immune system.
Diabetes and cardiovascular disease
Cardiovascular disease includes blood vessel disease, heart attack and stroke. It's the leading cause of death in Australia.
The risk of cardiovascular disease is greater for people with diabetes, who often have increased cholesterol and blood pressure levels. Smoking, having a family history of cardiovascular disease and being inactive also increase your risk.
To reduce your risk and pick up any problems early:
- Have your blood pressure checked at least every six months, or more often if you have high blood pressure or are taking medication to lower your blood pressure.
- Have your HbA1c checked at least every year, or three- to six-monthly if recommended.
- Have your cholesterol checked at least every year. Further pathology tests such as an electrocardiogram (ECG) or exercise stress test may also be recommended by your doctor.
Eyes and diabetes
Diabetes-related eye problems include:
- retinopathy – retinopathy is when blood vessels in the retina become damaged which eventually affects your vision. Retinopathy has various stages. In its early stages, there are usually no symptoms, so having a full diabetes eye check is essential to detect it early. Regular eye checks help detect any changes and allow for early treatment where needed to prevent further damage
- macular oedema – the macula is part of the retina and helps you to see things clearly. Swelling of this area can happen when the blood vessels in the retina are damaged, causing fluid to build up. This can lead to the macula being damaged and vision may become blurry. Treatment is available. Early detection is important
- cataracts – the lens of the eye becomes cloudy and can cause vision to become cloudy, distorted or sensitive to glare. People with diabetes can develop cataracts at an earlier age than usual
- glaucoma – the pressure of the fluid within the eye builds up to a higher level than is healthy. This pressure can damage the eye over time. Glaucoma occurs in people with and without diabetes, but is more common in people with diabetes.
While most people who have damage to the eyes have no symptoms in the earlier stages, there are certain symptoms that may occur and these need urgent review. If you have flashes of light, floaters, blots and dots or part of your vision missing, see your doctor immediately.
Regular eye checks
Everyone with diabetes should have a professional eye examination by an ophthalmologist or optometrist when they are first diagnosed, and then at least every two years after that (children usually start this screening five years after diagnosis or at puberty).
It is important that you inform the person checking your eyes that you have diabetes. If retinopathy or another abnormality is found, eye tests will be required every year, or more frequently if advised by your ophthalmologist.
Kidneys and diabetes
People with diabetes are at risk of kidney disease (nephropathy) due to changes in the small blood vessels of the kidneys. Kidney disease is painless and does not cause symptoms until it is advanced.
Screening is very important. Kidney damage can be diagnosed early by checking for microalbumin (very small amounts of protein) in the urine at least once a year. Your doctor will also check your kidney function, including estimated glomerular filtration rate (e-GFR), with a blood test.
If problems are picked up early, nephropathy can be slowed or prevented with the right treatment. Medicine called ACE inhibitors and angiotensin receptor antagonists help to protect the kidneys from further damage. These tablets can also be used to treat high blood pressure.
Nerves and diabetes
Nerve damage (neuropathy) is usually caused by high blood glucose levels, although similar nerve damage can also result from:
- drinking large amounts of alcohol
- vitamin B12 deficiency – long-term use of the diabetes medication Metformin (over three to five years) can increase the risk of vitamin B12 deficiency. Your doctor may test for this.
Damage can occur to the sensory (feeling) and motor (movement) nerves of the legs and feet, arms, hands, chest and stomach, and to the nerves that control the actions of body organs.
To help prevent nerve damage:
- Keep your blood glucose levels in target range.
- If you drink alcohol, keep within the recommended guidelines.
- Don't smoke.
- Talk to your doctor about any problems you have with your hands, arms, feet, or legs, your stomach, bowels, or bladder.
Feet and diabetes
The feet of someone with diabetes are at risk of damage when the blood supply in both large and small blood vessels is reduced. Nerve damage (peripheral neuropathy) often results and problems to the structure of the foot can also occur – for example, clawed toes.
Reduced blood supply and nerve function can delay healing, increase the risk of infection, reduce feeling in the feet, and lead to ulcers and structural foot problems.
Look after your feet by:
- seeing a podiatrist at least once a year. They will assess the health of your feet by checking the blood supply and nerve function and looking for changes in the structure of your feet
- checking your feet every day (get someone to help you if you are unable to check them yourself). Look for cuts, blisters, calluses, corns, tinea (especially between the toes) and any changes you notice. If treated early and without delay, you can help prevent complications occurring
- using a moisturiser (such as sorbolene), especially if you have areas of dry, rough or cracked skin on your feet and heels – this can help keep your feet healthy
- protecting your feet by wearing comfortable, supportive shoes that fit well.
Skin and diabetes
People with diabetes may experience very dry skin due to damage to the small blood vessels and nerves. A common problem for people with diabetes is very dry skin on the feet.
There are also other skin conditions related to diabetes. High blood glucose levels over time can affect the health of the skin. The skin acts as a barrier to protect our bodies from infection so it is important to keep the skin as healthy as possible. If the skin becomes dry, it can lead to cracks and possibly infections.
To reduce the risk of skin problems:
- Keep your blood glucose and HbA1c within recommended ranges to reduce the risk of skin infections.
- Wear gloves when you use household cleaners and solvents.
- Avoid very hot baths and showers.
- Do not have your feet too close to heaters, especially if you have peripheral neuropathy, as you may not be able to feel the intensity of the heat.
- Use a cream or lotion on your skin after bathing, preferably one that is not perfumed. Use non-scented soaps or soap alternatives.
- If you notice you have a skin problem, see your doctor.
Oral health and diabetes
People with poorly managed diabetes are at increased risk of tooth decay and gum infections. This is because the small blood vessels that help nourish your teeth and gums can become damaged. (Dental and gum infections can also lead to high blood glucose levels.)
Poor oral care can cause the gums to become inflamed and loosen around your teeth. It's also strongly linked with an increased risk of heart disease.
To reduce your risk of teeth and gum problems:
- See your dentist regularly (six monthly) for a check-up.
- Brush your teeth at least twice a day (a soft toothbrush is generally recommended) and floss once a day.
- If you have dentures, make sure you brush your dentures and gums with a soft toothbrush.
Mental health and diabetes
Living with and managing either type 1 or type 2 diabetes can lead to stress, anxiety and depression. This can affect your blood glucose levels and how you manage your diabetes in general. Over time, this can affect your health.
It is important to talk to your doctor if you are going through times of stress, depression or anxiety. Your doctor can refer you to a counsellor or psychologist by providing a diabetes mental health plan. This is Medicare rebated.
Other help is available, including:
- Tel. 13 11 14
- Beyond Tel. 1300 22 4636
- SANE Tel. 1800 18 7263
- Diabetes Victoria support services available throughout Australia and – NDSS Helpline 1300 136 588
- 1300 78 99 78
- Suicide call back 1300 659 467
- Black Dog online resources
Diabetes and infections
Your immune system helps to prevent and fight infection. High blood glucose levels slow down the white blood cells, which help fight infection. This makes it more difficult for the immune system to do its job.
Support your immune system and reduce your risk of infection by:
- keeping your blood glucose levels within the recommended range
- getting enough sleep each night
- washing your hands routinely, as needed
- having a yearly influenza (flu) immunisation
- asking your doctor about the pneumonia vaccine, especially if you are over 65
- seeing your doctor if you think you have an infection or are unwell.
Thyroid and diabetes
People with either type 1 or type 2 diabetes are at increased risk of thyroid disease. This includes both overactive and underactive thyroid. Thyroid disorders can affect general health and may affect blood glucose levels.
Thyroid function is assessed by a blood test. Talk to your doctor to see if you have had your thyroid function checked.
Sexual function and diabetes
Reduced blood supply and nerve damage can affect sexual function. Erectile dysfunction (impotence) in men is the persistent inability to achieve or maintain an erection sufficient for satisfactory sexual performance. This is a common problem for men of all ages and is more common in men with diabetes.
Erectile dysfunction is not a disease, but a symptom of some other problem – physical, psychological or a mixture of both. Most cases of erectile dysfunction are physical, such as nerve or blood vessel damage.
In women, sexual dysfunction is also reported, although there is a lack of research in this area. It is difficult to know whether this is directly related to hormonal changes such as menopause, or to diabetes.
It is important to seek help from your doctor, diabetes educator or organisations such as Healthy Male – Andrology .


taking care of yourself is the best we can do let's not stop walking let's exercise
You must be logged in to post a comment.